Laurie's Blogs.
Jan 2018
Guest Blog - LLLT/PBM vs Active Epiphyses

by Peter A Jenkins, MBA
A frequently-recurring question regarding the clinical use of Laser Therapy is whether treating over active epiphyses is contraindicated.
The general list of contraindications to Low-Level Laser Therapy (LLLT) – now, formally, Photobiomodulation (PBM) – in physiotherapy has largely been carried over from other active modalities, such as ultrasound and e-stim, and accepted without question and with an overabundance of caution, as applying to laser therapy in general.
The use of laser over or near the active epiphysis seems – originally, at least – to have fit this category; it is often listed in device operating manuals and by clinical educators in various fields as being contraindicated, but it is also, equally, stated by others (myself included) to be of no great concern.
What is the real story?
In 2010 the Canadian Physiotherapy Association published ‘ELECTROPHYSICAL AGENTS Contraindications and Precautions: An Evidence-Based Approach to Clinical Decision Making in Physical Therapy’(1). According to this document, LLLT/non-coherent light is considered to be safe to use “on skin overlying active epiphysis”, and “can be applied with caution” to the active epiphysis.
To my knowledge, this is the first – and, possibly, only – formal guidance document of this type to address the safety of Low Level Laser Therapy/Photobiomodulation in an evidence-based manner, and its recommendations for physiotherapists were, contemporaneously, accurate and well-founded. However, not all the recommendations are, necessarily, applicable to other specialties, nor – as we’ll now see – is the recommendation about epiphyses still current.
I conducted a search of PubMed, Google Scholar, ResearchGate, and a number of laser- and photobiomodulation-related Journal websites and texts, for various combinations of the key words ‘laser’, ‘laser therapy’, ‘LLLT’, ‘photobiomodulation’, ‘PBM’, ‘epiphysis’, ‘epiphyses’, ‘epiphyseal’, and ‘growth plate’, and turned up relatively few relevant articles (2-11), one indirectly relevant paper (12), and a number of false positives. Two of these false positives (13, 14) are often, inappropriately, cited in lay discussion as ‘evidence’ of the negative impact of laser therapy on active epiphyses.
When the CPA document was published in 2010, the only readily-available literature was that regarding a study by Cheetham et al, 1992(2) in which the effects of laser therapy over active epiphyses were investigated. In 2002, Navratil et al(3) referred to this study when stating that “the fear of possible damage to the epiphyseal slots in children in the case of the application of therapeutic laser is baseless”. Other work(4,5) had been done at the time, but accessibility of the literature was limited due to it having only been published in the Russian language.
In the years since 2010, six more directly-relevant papers (6-11) have been published, along with another(12) that contains pertinent information, albeit from within a different field. The various studies shed more light on the effects of LLLT/PBM on epiphyseal growth, but the results remain somewhat controversial.
For example, de Andrade(8) and Handayani(11) found no significant effects on the histology of the epiphyseal cartilage or the final length of limbs, but Cressoni(7) showed that laser irradiation may improve cartilage structure in rats, while Seifi(6), Oliveira(9) and Yeom(10) all found significant histological and histomorphometric changes, particularly within the hypertrophic zone, and changes in bone length. Oliveira(9) found that the femoral longitudinal length decreased, whereas Yeom(10) found an increased rate of growth. And, while investigating the impact of photodynamic therapy upon epiphyseal plates, Kurchenko(12) found that laser irradiation without the introduction of a photosensitiser led to intracellular swelling of epiphyseal plates chondrocytes.
A major confounding factor, when considering these findings in relation to our initial question, is that each of these studies was conducted with widely differing device and treatment parameters, and the devices used bear scant resemblance to any currently in clinical use.
Where reported, the ‘stationary contact’ application technique was consistent among all studies, but the number of points irradiated and the number of irradiations performed over time varied greatly. Output powers ranged from 4 to 100 mW, power densities from 2 to 563 mW/cm2, irradiation durations from 8.5 secs to 8 minutes, wavelengths from 635 to 904 nm, and dosimetry was all over the shop! (Table 1. Parameters)
Essentially, there is little basis for meaningful comparison of these studies, other than they were investigating effects upon similar tissues by applying laser light to similar anatomical locations.
Two studies(10, 11) treated acupuncture points, rather than specific anatomical locations over the growth plates. However, two of the points used – ST36 and SP6 – are located adjacent to growth plates; ST36 about 1 mm lateral of the tibial tuberosity, and SP6 a few mm above the medial malleolus on the posterior border of the medial aspect of the tibia. Perhaps unsurprisingly, irradiation over these points elicited greater changes than irradiation of GV20, which is located at the peak of the head, midpoint of a line connecting the apexes of the two auricles. (Figure 1)
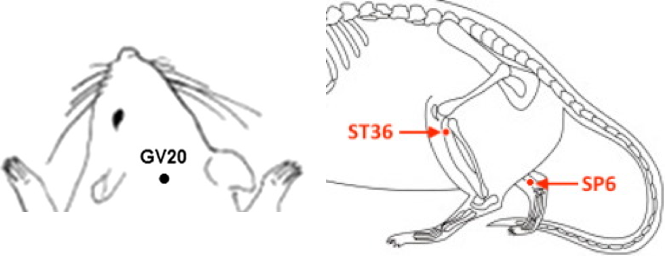
Figure 1. Acupoints GV20, ST36 and SP6 on the rat
Although some studies found no effects of laser irradiation – at the parameters used – upon active epiphyses in rats and hamsters, others did, so there is certainly evidence of effects such as increased angiogenesis, increased proliferation of chondrocytes, and increased calcification.
Not all of the potential effects of LLLT/PBM on growth plates are, necessarily, negative. Yeom et al(10), for example, conclude that longitudinal bone growth induced by laser acupuncture [to points directly over growth plates] “may have a clinical potential in promoting longitudinal bone growth in children”, and Seifi et al(6) suggest that “laser irradiation with the chosen parameters can stimulate condylar growth and subsequently cause mandibular advancement […] for further improvement of mandibular retrognathism”. Mavrich and Luzin(4) state that that laser can be used for the optimisation of growth, mineralization and stability of skeleton bones.
Where does this leave us?
Even with these new data, it is only clear that there is still no clear answer to our question. Yes, there is evidence of effects of LLLT/PBM upon active epiphyses, and in some cases, this may prove to be strongly contraindicated. What is not addressed by any these studies, however, is the relative benefit or otherwise of utilising LLLT/PBM in young patients versus withholding treatment due to concerns over the impact to growth plates; what’s best for each patient must take priority, and there is bound to be many instances where, despite any possible risks, LLLT/PBM is strongly indicated. In all cases, therefore, a cautious and well-considered approach is recommended.
With more information, we can make better-informed clinical choices, although, with the current data, it is not possible to determine an upper or lower margin for any of the important parameters, nor to accurately define a ‘window’ of effect.
However, and if one doesn’t look too closely at the weeds and seeds, it might be possible to find a ‘big picture’ pattern among the data suggesting that (a) more frequent treatments with higher intensities and/or doses over longer periods are more likely to have deleterious effects, than (b) less-frequent treatments with lower intensities/doses over shorter periods. It is worth noting, too, that no studies have yet considered the effect of high-powered (i.e. Class 4 or IV) ‘therapeutic’ lasers and/or very high doses.
NB. I have not made any general statements about a ‘safe’ or otherwise number of J/cm2, as this is a relatively meaningless number in terms of its relevance clinical effects. The failings of J/cm2, and the importance of reporting and considering other parameters, will be addressed in a future article.
References:
- Physiotherapy Canada (2010) ELECTROPHYSICAL AGENTS Contraindications and Precautions: An Evidence-Based Approach to Clinical Decision Making in Physical Therapy V62/5 Special Issue.
- Cheetham MJ, Young SR, and Dyson M. (1992) Histological effects of 820 nm laser irradiation on the healthy growth plate of the rat. Laser Therapy, vol. 4, no. 2, pp. 59–63.
- Navrátil L and Kymplova J. (2002) Contraindications in noninvasive laser therapy: truth and fiction. J. Clin. Laser Med. Surg. 20, 341–343.
- Mavrich VV, Luzin VI. (2000) The growth, chemical composition and strength properties of the long tubular bones in the skeleton of white rats under the influence of low energy laser radiation. Morfologiia. 2000;117(1):59-66. [Article in Russian]
- Pereslytskikh PF (2008) Formation of ossification nucleus in the femoral head in hamsters exposed to laser radiation. Morfologiia. 2008;134(6):68-72. [Article in Russian]
- Seifi M, Maghzi A, Gutknecht N, Mir M, Asna-Ashari M. (2010) The effect of 904 nm low level laser on condylar growth in rats. Lasers Med Sci. 2010;25(1):61-5.
- Yeom M, Kim S-H, Lee B, Zhang X, Lee H, Hahm D-H, Sohn Y, Lee H. (2013) Effects of Laser Acupuncture on Longitudinal Bone Growth in Adolescent Rats. Evidence-Based Complementary and Alternative Medicine: eCAM, 2013, 424587.
- Cressoni MDC, Giusti HHKD, Piao AC, de Paiva Carvalho RL, Anaruma CA and Casarotto RA. (2010) Effect of GaAlAs laser irradiation on the epiphyseal cartilage of rats. Photomedicine and laser Surgery, 28(4), pp.527-532.
- de Andrade AR, Meireles A, Artifon EL, Brancalhão RMC, Ferreira JRL and Bertolini GRF. (2012) The effects of low-level laser therapy, 670 nm, on epiphyseal growth in rats. The Scientific World Journal, 2012.
- de Oliveira SP, Rahal SC, Pereira EJ, Bersano PRD, Vieira FD, and Padovani CR. (2012) Low-level laser on femoral growth plate in rats. Acta Cirurgica Brasileira, vol. 27, no. 2, pp. 117–122, 2012.
- Handayani S, Ramelan AH, Purwanto B, Saputra K and Tamtomo DG (2017) Histology of Epiphyseal Plate of Adolescent Rat Stimulated by Laserpuncture J. Phys.: Conf. Ser. 909 012092
- Kurchenko S, Shashko A, Dudin M, Mikhailov V, Netylko G, Ashmarov V. (2012) Photodynamic impact on the epiphyseal plates. Stud Health Technol Inform. 2012;176:174-8.
- Morein G, Gassnerb S, and Kplanc I. (1978) Bone growth alterations resulting from application of CO2 laser beam to the epiphyseal growth plates: an experimental study in rabbits. Acta Orthopaedica Scandinavica, vol. 49, no. 3, pp. 244–248, 1978.
- Peterson HA and Wood MB. (2001) Physeal arrest due to laser beam damage in a growing child. J. Pediatr. Orthop. 21, 335–337.
Author’s Biography
Peter A. Jenkins, MBA, began his exciting and ongoing adventure in the world of laser therapy & photobiomodulation in Australia in 1996. His technical background includes the specification and development of laser devices for safety, reliability, affordability and efficacy, and he is driven to create technologies that enable practitioners to optimize their patients’ clinical outcomes. A passionate educator, and co-author of a number of peer-reviewed articles, Peter sees market education as the key to improving standards in the laser therapy/photobiomodulation industry and holding manufacturers and marketers accountable for the claims they make.
Professional Positions
- Spectra-Medics Pty Ltd (Founder, Managing Director)
- SpectraVET, Inc. (Co-Founder, Dir. Education & Technology)
- Immunophotonics, Inc. (Co-Founder, Technology Advisor)
Honorary Positions
- Co-Founder & Council Member, Australian Medical Laser Association Inc
- Co-Founder, Co-Editor, The Annals of Laser Therapy Research
- Committee Member, Standards Australia HE3-12/003 (Medical Laser Safety)
- Peer Reviewer, Photomedicine & Laser Surgery
- Peer Reviewer, Lasers in Surgery & Medicine
- Peer Reviewer, Photochemistry & Photobiology
- Peer Reviewer, Dose-Response
- Past President (1998-9), Hornsby and District Chamber of Commerce & Industry Inc
Qualifications
- Master of Business Administration (University of Western Sydney) 1997
- Avionics Technician (Royal Australian Air Force) 1992
- Instrument Fitter (Royal Australian Air Force) 1984